March/April Issue of Vein Specialist
Superficial Venous Session at VENOUS2023

Christine Shokrzadeh, MD, FACS, RPVI
University of Texas Medical Branch

Daniel Monahan, MD, FACS
Monahan Vein Clinic
Roseville, CA
The Superficial Venous Session on Thursday of the Annual Meeting included a potpourri of topics. State-of-the-art talks were given by Dr Kathy Gibson on use of various ablation technologies and Dr Steve Elias on the essentials of clinical evaluation and ultrasound of the venous patient. New research was presented on a range of topics including payor coverage policies; hemodynamics hindering durable treatment outcomes, location of varices as a factor in treatment success,; comparison of polidocanol foam vs RFA in ablation results; safety of ablation procedures in patients with a prior DVT; whether length of treated GSV affects patient reported outcomes; safety and efficacy of ultrasound-guided foam sclerotherapy; and a complicated case of superficial venous phlebitis discussed by Dr Julianne Stoughton. Several presentations analyzed VQI database content to delineate clinically useful information on treating vein patients. Basic state of practice knowledge was shared along with pointers toward the future. The program content presented was engaging and practical for new and experienced specialists treating superficial venous disease.

Poster Session: A Bigger-than-Texas Success!

Nasim Hedayati, MD
Co-Chair, VENOUS2023 Poster Session
Member, AVF Early Career Committee
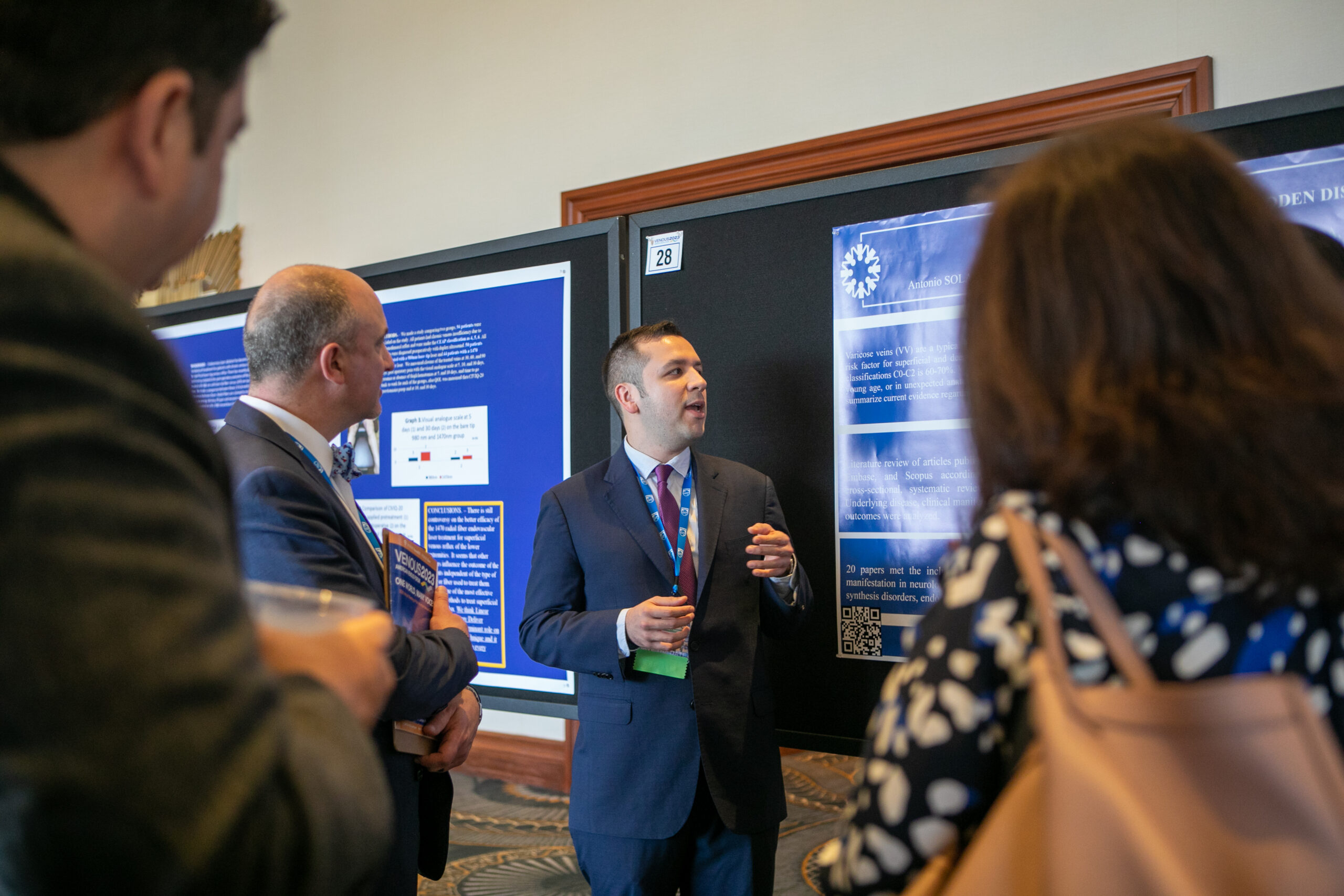
Dr Antonio Solano presenting his poster to the judges.
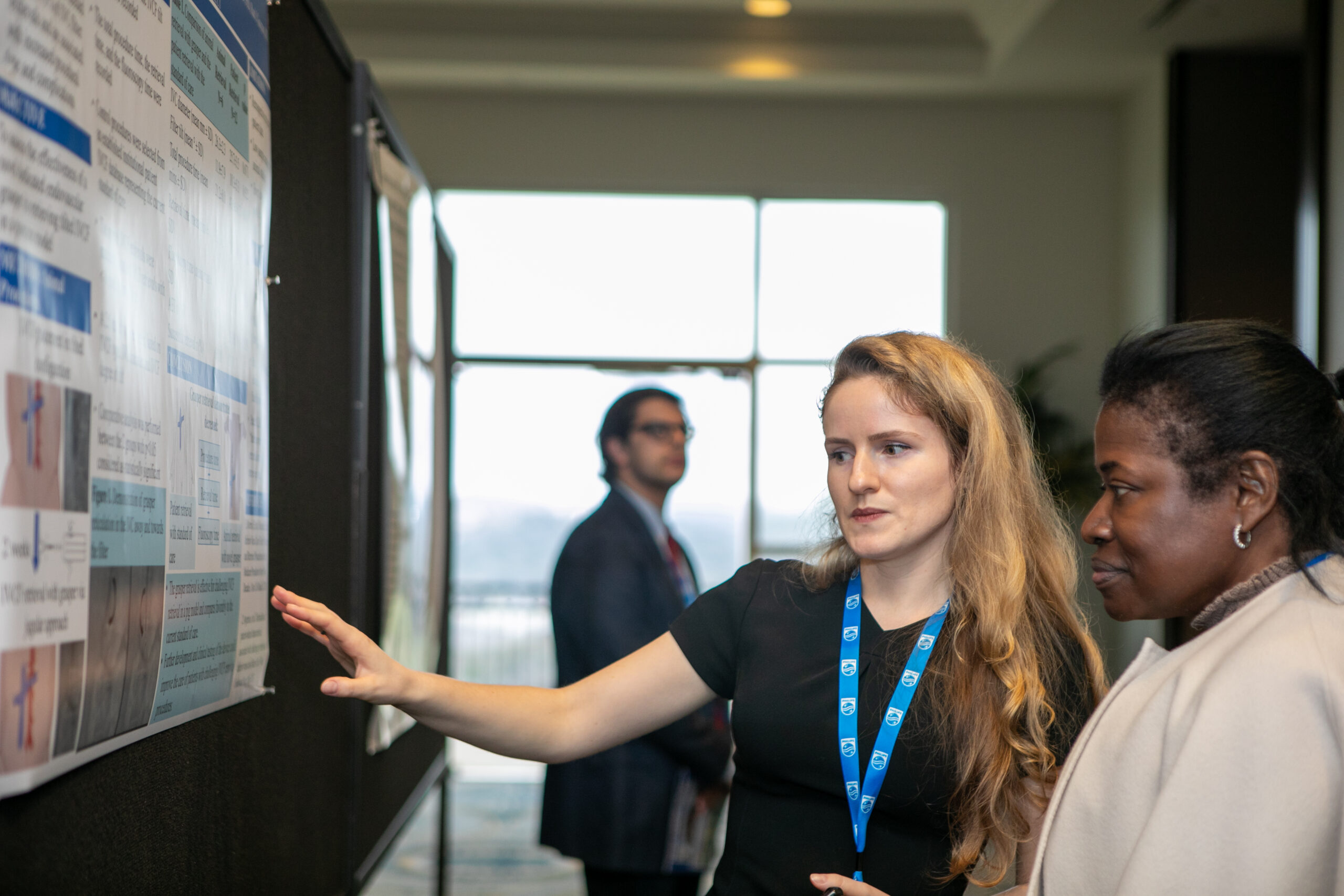
Everything is bigger and better in Texas, and the poster session was no exception! With more than 50 posters from the United States, Europe, and South America, we can say this year’s session will go down in history as one of our best. The quality of the presentations, topics, and data presented was truly outstanding. We had medical students, surgical residents and fellows, industry members, seasoned investigators, and AVF members presenting their work. In addition to the presenters, we would like to thank the judges who made this fiesta a grand success.
Judging these posters was certainly not an easy task. The winner of the poster competition was, “An Updated Systematic Review and Meta-analysis of the Additional Benefit of Graduated Compression Stockings to Pharmacologic Thromboprophylaxis in the Prevention of Venous Thromboembolism in Surgical Inpatients from London, England.” The authors were: Benedict Turner, MBChB, BSc, FHEA, Sara Jasionowska, MBBS, BSc, FHEA, Matthew Machin, MBBS, BSc, FHEA, Joseph Shalhoub, MBBS, PhD, FRCS, FEBVS, and Alun Davies, DSc, PhD, FRCS. The presenters discussed their work on the question of necessity of compression stockings in the postoperative setting. The question answered could potentially save hundreds of thousands of healthcare dollars.
In second place was, “Preoperative VCSS Pain, Varicose Veins, and Pigmentation are Significant Predictors of Major Re-operation.” The authors were Halbert Bai, MPH, Jason Storch, BA, Jenny Chen, BA, Jerry Zhu, BS, Kevin Chun, BA, Anna Williams, Jinseo Kim, Yeju Kang, and Windsor Ting, MD from Icahn School of Medicine at Mount Sinai.
The poster session allowed for small personal interactions among the judges and authors in a semiformal setting. This year’s session was a huge success! Thank you to the program committee, American Venous Forum’s leadership, and administrative staff for bringing this event to our annual conference.
Until next year, thank you to all the participants and supporters of this session! See ya’ll in Florida!
Exploring the Depths of Deep Venous Disease

Paula Pinto Rodriguez
Research Fellow, Division of Vascular Surgery and Endovascular Therapy, Department of Surgery, Yale School of Medicine

Cassius Iyad Ochoa Chaar, MD, MS
Associate Professor in Surgery, Yale School of Medicine
The deep venous session of VENOUS2023 was a highly informative event that brought together experts in the field. The session featured 9 plenary talks covering various topics related to deep venous interventions and highlighting the complex interplay of deep venous reflux and obstruction. Dr Mariza Lugli from Hesperia Hospital in Italy opened the session by presenting an overview of techniques for deep venous valve repair. The speaker highlighted 3 techniques: vein transposition, valve transplant, and neovalve, and shared the outcomes of the large experience of her center. She emphasized the importance of a strict diagnostic protocol and adequate patient selection to achieve good outcomes. Later, Dr Jorge Ulloa from the University of Los Andes in Columbia delivered the 3-year outcomes of a first-in-human trial that addresses the same clinical problem with a novel bioprosthetic venous valve. The results showed that clinical outcomes were very good with improvements in venous reflux of 63%, rVCSS of 64%, and VAS of 83% after 36 months. Both speakers highlighted the need to establish an appropriate modality for measuring treatment response since reflux measurement persisted in a significant portion of patients despite clinical improvement.
Dr Karem Harth, from University Hospitals in Cleveland, discussed the landscape of venous stent usage and clinical indications for stenting. She emphasized the significant increase in venous stenting following the FDA approval highlighting the need for further research to understand the suitability of venous stent usage and to ensure these devices are used equitably across the population. Despite the growing use of venous stenting, minimal consensus exists on the optimal type and duration of antithrombotic therapy after these procedures. A study performed at the University of Pittsburgh Medical Center and presented by Dr Nishant Agrawal concluded that initiating early antiplatelet treatment up to 30 days after stenting in patients with non-thrombotic iliac vein lesions and post-thrombotic syndrome was associated with a significantly reduced risk of stent failure at 1 year. However, further research is needed to establish the optimal type and duration of antithrombotic therapy after venous stenting. Jason Storch, a medical student at the Icahn School of Medicine at Mount Sinai New York, presented an institutional series lead by Dr Windsor Ting highlighting the differences in outcomes of iliac vein stenting for outflow obstruction between different age groups. Older patients presented with more severe disease, but were more likely to have complete resolution of symptoms after iliac vein stenting compared to younger patients who were more likely to undergo minor reinterventions.
Dr Erin Murphy from Atrium Health ended the session by sharing technical tips in deep venous stenting around the femoral vein and highlighted the importance of preserving adequate inflow through the profunda vein with endovascular or open surgical techniques. The audience was very excited about the various presentations and engaged in lively discussions. Overall, the deep venous session of VENOUS2023 provided attendees with a wealth of knowledge and insights into the latest developments in the field of deep venous disease. The diverse range of topics and backgrounds of the speakers highlighted the quality of the science that the American Venous Forum offers in its annual meeting.