May/June Issue of Vein Specialist
Pneumatic Compression Makes Everyday Joys Possible

Jennifer Heit, PT, DPT, CLT-LANA
Tactile Medical
Phlebolymphedema, or lymphedema associated with chronic venous insufficiency (CVI), is the most common cause of secondary lymphedema in the United States,1 although under-recognized and undertreated. Phlebolymphedema can have significant effects on quality of life for people experiencing this chronic, progressive condition. It can cause pain, impaired mobility, increased risk for infection, and make the everyday joys like walking a dog, playing with kids or grandkids, or wearing favorite shoes seem out of reach.
Phlebolymphedema begins with venous hypertension, which increases microfiltration from arterioles, leaving the lymphatic system with excess fluid to collect and transport from the interstitial space. Over time the lymphatic system can become overwhelmed and damaged, leading to stagnated protein-rich fluid in the interstitium, which is associated with increased risk for cellulitis and skin changes such as fibrosis. Other skin changes associated with phlebolymphedema can include hyperkeratosis, hemosiderin staining, or even progression to venous ulcers. While many patients rightfully receive treatment of the veins in this situation, often lymphatic-specific treatment is lacking when swelling persists after vascular interventions.
One tool patients can use to effectively manage lymphedema at home is pneumatic compression. While many pneumatic pump choices exist for clinicians and patients, features and benefits vary, so it is important to choose appropriately. For example, an advanced pneumatic compression device like the Flexitouch® Plus from Tactile Medical uses dynamic pressure, which means that chambers of the garments inflate and deflate sequentially creating a wave-like motion that directs fluid out of the lower extremities toward areas of the body with a healthy lymphatic system–similar to how a certified lymphedema therapist performs manual lymphatic drainage. It is also the most clinically researched device, with studies showing effects such as significant limb volume reduction, reduction in total lymphedema-related costs, decreased cellulitis episodes, and improved ability for patient to perform activities of daily living.2,3
Kelly is a veteran who had chronic swelling and draining of his legs due to lymphedema, which impacted his ability to get around like he wanted. He thought he tried everything to stop the draining until eventually the VA clinic was able to help him obtain the Flexitouch® to use at home. Kelly reported, “Within 5 days I quit draining.” One of his everyday joys is taking his dog to the park, which he was able to do again after adding pneumatic compression to his lymphedema management routine at home. In Kelly’s words, “It’s a life saver; it really is you know one of those things that allows you to live a normal life instead of a life that’s compromised from lymphedema.”
Watch Kelly’s full story here.
Disclosure: Jennifer Heit serves as a Senior Clinical Specialist for Tactile Medical.

Kelly O, a veteran who lives with lymphedema, uses pneumatic compression as a component of daily management.
References
- Dean SM, Valenti E, Hock K, Leffler J, Compston A, Abraham WT. The clinical characteristics of lower extremity lymphedema in 440 patients. J Vasc Surg Venous Lymphat Disord. 2020; 8(5):851-859.
- Muluk SC, Hirsch AT, Tafe EC. Pneumatic Compression Device Treatment of Lower Extremity Lymphedema Elicits Improved Limb Volume and Patient-Reported Outcomes. EJVES. 2013; 46(4): 480–487.
- Karaca-Mandic P, Hirsch AT, Rockson SG, Ridner SH. The Cutaneous, Net Clinical, and Health Economic Benefits of Advanced Pneumatic Compression Devices in Patients with Lymphedema. JAMA Dermatol. 2015;151(11):1187–1193.
A New Treatment Choice
That Keeps Patients Living Life

Maggie Thompson
Senior Vice President
Payer Strategy and Operations
KOYA Medical

Charles Liu
Chief Marketing Officer
Koya Medical
Patients with lower limb lymphedema are frequently seen in the vascular clinic. While this condition has been ascribed to a variety of causes over the years, a recent studyhas shown that the leading cause stems from underlying venous disease.1Phlebolymphedema is lymphedema (LED) developed as a result of chronic venous insufficiency (CVI). CVI or venous stasis and LED lead to a decrease in quality of life, impaired mobility, and a higher incidence of lower extremity wounds and associated morbidity.2 A 2022 consensus among expert practitioners who treat both LED and CVI concluded that lymphedema treatment is appropriate for patients with CEAP 3 and greater.3 Multiple modalities are utilized in treating phlebolymphedema, much of it occurring outside of the clinic, including elevation of limb in the earlier stages and use of compression stockings and pneumatic compression device (PCD) in later stages. Introduced in the 1950s,4 PCDs compress by pumping air into separate chambers. This treatment has been shown to be effective, but their use is limited by the need for a fixed power source and consequent restriction of patient mobility, and hence limiting the effect of the calf-muscle pump function in clearing fluid from the interstitium.5
In 2021, FDA approved Dayspring® (Koya Medical), a non-pneumatic compression device (NPCD), bringing a novel and effective approach that draws on multiple, well-established compression principles, and integrates them to deliver a patient friendlier treatment in a single session. Dayspring NPCD is multimodal, providing static compression (similar to that provided by compression garments), gradient sequential compression, and allowance for exercising muscle and joint contractions. While these various individual approaches are often cited and recommended in the various clinical guidelines,6 no single treatment option existed until Dayspring NPCD provided the means or opportunities for which they can be accomplished simultaneously. The unique combined aspect of this treatment is especially important in the calf, which is responsible for the majority of the venous return, with both a high capacitance and an ejection fraction of 65%.7 Patients with venous reflux develop symptoms because the rate of venous flow exceeds the output of the calf. Ambulation increases the ejection fraction and thus overall venous return. Further, the compact nature and portability of Dayspring with its mobile power source allows the patient to be and remain mobile so they may address their basic daily living activities—a preference stated by patients. 8,9 In contrast, PCDs are typically not as portable, much bulkier, and the treatment’s requirement due to the need to be affixed to a stationary power source may play a role in deterring usage. (Figure 1)
Multiple studies 8,9 have been conducted investigating the clinical utility and comparative effectiveness of Dayspring NPCD compared to advanced PCDs (APCDs). In the most recent randomized, multi-center, prospective cross-over study, topline results showed that Dayspring significantly outperformed APCDs in terms of lower extremity limb volume reduction, improvement in quality of life, and adherence.
CMS recognizes Dayspring as a distinctive technology and awarded unique HCPCS codes to the Dayspring device, rather than using existing PCD codes (Table 1).
| Controller | E0680—Non-pneumatic compression controller with sequential calibrated gradient pressure |
| Garments/Appliances | E0682—Non-pneumatic sequential compression garment, full arm E0678—Non-pneumatic sequential compression garment, full leg E0679—Non-pneumatic sequential compression garment, half leg |

Dayspring NCPD treatment*

Typical PCD treatment
References
- Dean SM, Valenti E, Hock K, Leffler J, Compston A, Abraham WT. The clinical characteristics of lower extremity lymphedema in 440 patients. J Vasc Surg Venous Lymphat Disord. 2020;8(5):851-859. doi: 10.1016/j.jvsv.2019.11.014. Epub 2020 Jan 25. PMID: 31992537.
- James C, Park SY, Chan M, Khajoueinejad N, Alabi D, Lee J, Lantis JC 2nd. The Role of Intermittent Pneumatic Compression in the Treatment of Lower Extremity Chronic Wounds. Surg Technol Int. 2021;38:79-86. doi: 10.52198/21.STI.38.WH1417. PMID: 33765323.
- Lurie F, Malgor RD, Carman T, Dean SM, Iafrati MD, Khilnani NM, Labropoulos N, Maldonado TS, Mortimer P, O’Donnell TF Jr, Raffetto JD, Rockson SG, Gasparis AP. The American Venous Forum, American Vein and Lymphatic Society and the Society for Vascular Medicine expert opinion consensus on lymphedema diagnosis and treatment. Phlebology. 2022;37(4):252-266. doi: 10.1177/02683555211053532. Epub 2022 Mar 8. PMID: 35258350; PMCID: PMC9069652.
- Brush BE, Heldt TJ. A device for relief of lymphedema. JAMA. 1955;158(1):34-5. doi: 10.1001/jama.1955.02960010000009. PMID: 14367033.
- Greenall R, Davis RE. Intermittent pneumatic compression for venous thromboembolism prevention: a systematic review on factors affecting adherence. BMJ Open. 2020 Sep 3;10(9):e037036.
- O’Donnell TF Jr, Allison GM, Iafrati MD. A systematic review of guidelines for lymphedema and the need for contemporary intersocietal guidelines for the management of lymphedema. J Vasc Surg Venous Lymphat Disord. 2020;8(4):676-684. doi: 10.1016/j.jvsv.2020.03.006. Epub 2020 May 20. PMID: 32444277.
- Meissner MH. Lower Extremity Venous Anatomy. Semin Interv Radiol. 2005;22(3):147–56.
- Rockson SG, Whitworth PW, Cooper A, Kania S, Karnofel H, Nguyen M, Shadduck K, Gingerich P, Armer J. Safety and effectiveness of a novel nonpneumatic active compression device for treating breast cancer-related lymphedema: A multicenter randomized, crossover trial (NILE). J Vasc Surg Venous Lymphat Disord. 2022 10(6):1359-1366.e1. doi: 10.1016/j.jvsv.2022.06.016. Epub 2022 Aug 8. PMID: 35952956.
- Rockson SG, Karaca-Mandic P, Nguyen M, Shadduck K, Gingerich P, Campione E, Hetrrick H. A non-randomized, open-label study of the safety and effectiveness of a novel non-pneumatic compression device (NPCD) for lower limb lymphedema. Sci Rep. 2022 17;12(1):14005. doi: 10.1038/s41598-022-17225-9. Erratum in: Sci Rep. 2023 Jan 17;13(1):911. PMID: 35977981; PMCID: PMC9385615.
The geko™ device:
Breakthrough Technology for Post-Operative Care and Management of Venous Disease

Kieron Day, MD
Head of Clinical Affairs
Geko
In the realm of medical innovation, advancements often emerge from unexpected quarters. The geko® device, a small neuromuscular electrostimulation device, is an example of how technology can transform healthcare in profound ways. Originally developed for applications in sport recovery, the geko has found its niche in healthcare, particularly in enhancing blood flow and addressing various vascular conditions. In this article, we delve into how the geko device is revolutionizing post-operative care, preventing venous thromboembolism (VTE), reducing edema, and offering relief to patients suffering from venous leg ulcers.

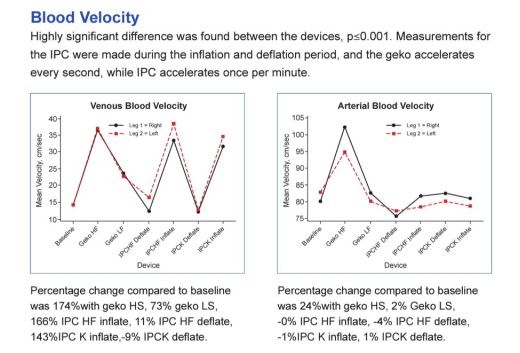
One of the primary mechanisms through which the geko exerts its therapeutic effects is by enhancing blood flow in the deep veins of the leg.1 This is achieved through neuromuscular electrostimulation, which activates the calf and foot muscle pumps, mimicking the natural physiological mechanism of walking. By stimulating the peroneal nerve, the device triggers muscle contractions, significantly increasing venous return and arterial inflow – at a rate equal to 60% of walking.2 This enhanced blood flow is crucial in various clinical scenarios, particularly in preventing the formation of blood clots which are significant risks following surgery or periods of immobility.3
Venous thromboembolism (VTE) is a major concern in hospitalized and at-home patients after a major surgical and non-surgical procedure.3 The geko offers a non-invasive solution to mitigate this risk. By promoting blood flow without the need for external compression, the device significantly reduces the likelihood of thrombus formation.1 This not only enhances patient safety and compliance but also alleviates the burden on healthcare resources associated with managing VTE complications.
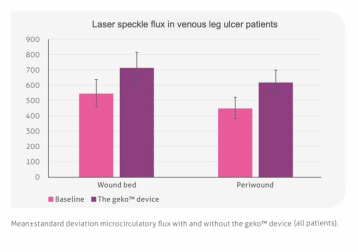
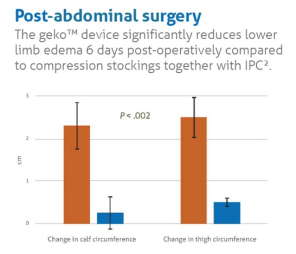
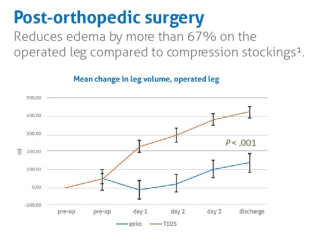
Edema is a common post-operative complication and a challenge in managing venous disease. ie, venous leg ulcers.4 The geko device plays a pivotal role in edema management through its ability to enhance lymphatic drainage and reduce fluid accumulation. By stimulating muscle contractions, the device facilitates the movement of lymphatic fluid, aiding in the clearance of excess interstitial fluid. This not only helps alleviate discomfort and improve ulcer healing but also reduces the risk of secondary complications such as infection.5
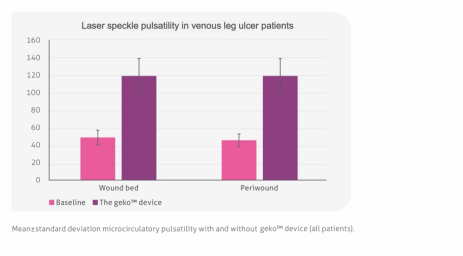
Venous insufficiency, a condition characterized by impaired venous return, often manifests as venous leg ulcers—a chronic and debilitating complication affecting millions worldwide. The geko offers a multifaceted approach to managing venous disease by addressing underlying vascular insufficiency5. By enhancing blood flow and reducing edema, the device improves tissue perfusion and oxygenation, essential for the healing process in both venous and peripheral arterial disease (PAD). 6 Additionally, its ability to stimulate muscle contractions aids in calf muscle pump function, further enhancing venous return and reducing venous hypertension.7
The geko represents a paradigm shift in post-operative care and the management of vascular conditions such as chronic venous insufficiency and venous leg ulcers. Its ability to enhance blood flow,2 prevent VTE,1 reduce edema,8 and address venous insufficiency5 makes it a valuable tool in the armamentarium of healthcare professionals. As technology continues to evolve, innovations like the geko hold the promise of improving patient outcomes, enhancing quality of life, and reducing healthcare costs.
References:
- Nicolaides A, Griffin M. Measurement of blood flow in the deep veins of the lower limb using the geko™ neuromuscular electro-stimulation device. International Angiology2016;35(4):406-10.
- Tucker A, et al. Augmentation of venous, arterial, and microvascular blood supply in the leg by isometric neuromuscular stimulation via the peroneal nerve. Int J Angiol. 2010; 19(1): e31–e37. doi: 10.1055/s-0031-1278361
- Prasad A. et al. Leg Ulcers and Oedema: A Study Exploring the Prevalence, Aetiology, and Possible Significance of Oedema in Venous Ulcers. Sage Journals. Volume 5, Issue 3https://doi.org/10.1177/026835559000500306
- Bull RH, Clements D, Collarte AJ, Harding KG. The impact of a new intervention for venous leg ulcers: A within-patient controlled trial. Int Wound J. 2023; 20(6): 2260–2268. doi:1111/iwj.14107
- Williams J, et al. The use of a novel neuromuscular electrical stimulation device in peripheral vascular disease. Int J Case Rep Images2014;5(11):744–747. doi:10.5348/ijcri-201462-CS-10048.
- Williams J, et al. The calf muscle pump revisited. J Vasc Surg Venous Lymphat Disord. http://dx.doi.org/10.1016/j.jvsv.2013.10.053
- Mahmood I, et al. Neuromuscular Electrostimulation Device Reduces Preoperative Edema and Accelerates Readiness for Theater in Patients Requiring Open Reduction Internal Fixation for Acute Ankle Fracture. Techniques in Foot & Ankle Surgery2019