What is Vein Disease?
Find relevant information here.
What Is Iliac Vein Compression Syndrome (May-Thurner Syndrome)?
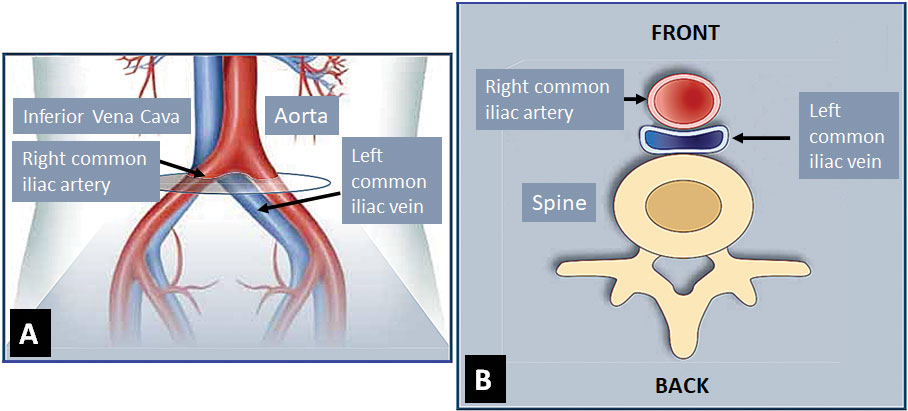
Iliac vein compression syndrome, also called May-Thurner syndrome, is caused by anatomic compression of the veins in the pelvis (iliac veins), which reduces blood return from the legs. The iliac veins carry blood from each leg into the abdominal cavity, and join to form the inferior vena cava, which then returns the blood to the heart. The iliac veins are located behind the iliac arteries and in front of the spine. In some people, the right iliac artery rests over the left iliac vein, compressing it between the artery and the spine. Examples of other causes of iliac vein compres include tumors or scarring.
- An illustration of the right common iliac artery crossing the left common iliac vein as blood flow from the aorta, lying to the left of the vena cava, goes to the right leg. B. Cross sectional drawing showing that the arty crosses on top of the vein just as the two vessels overlap the spine in the back (©Becton Dickinson. Used with permission) (The Healthy Veins Book, 2023, p. 179, fig. 34-2).
What are the Symptoms of Iliac Vein Compression Syndrome?
Most commonly, people notice swelling in one or both legs. People may also have varicose veins of the affected leg, leg tiredness, heaviness or fullness, and sometimes symptoms of low back or pelvic pain or fullness. The symptoms of the iliac vein compression syndrome often overlap with those of lower extremity venous disease or pelvic congestion syndrome.
How is Iliac Vein Compression Syndrome Diagnosed?
Your physician or non-physician provider will first ask you questions about your symptoms, other parts of your medical history, and perform a physical exam. Often, an ultrasound is ordered to look at the leg veins which may suggest the presence of venous disease in the pelvis. Additional ultrasounds specifically looking at the veins in the pelvis may need to be performed. These ultrasounds often require you to be fasting so that bowel gas doesn’t obstruct the view of the veins. Your physician or non-physician provider may request a CT scan or MRI to be able to assess these blood vessels better. Finally, they may decide to perform a venogram, which uses contrast dye, x-rays, and minimally invasive interventions to detect compression.
How is Iliac Vein Compression Syndrome Treated?
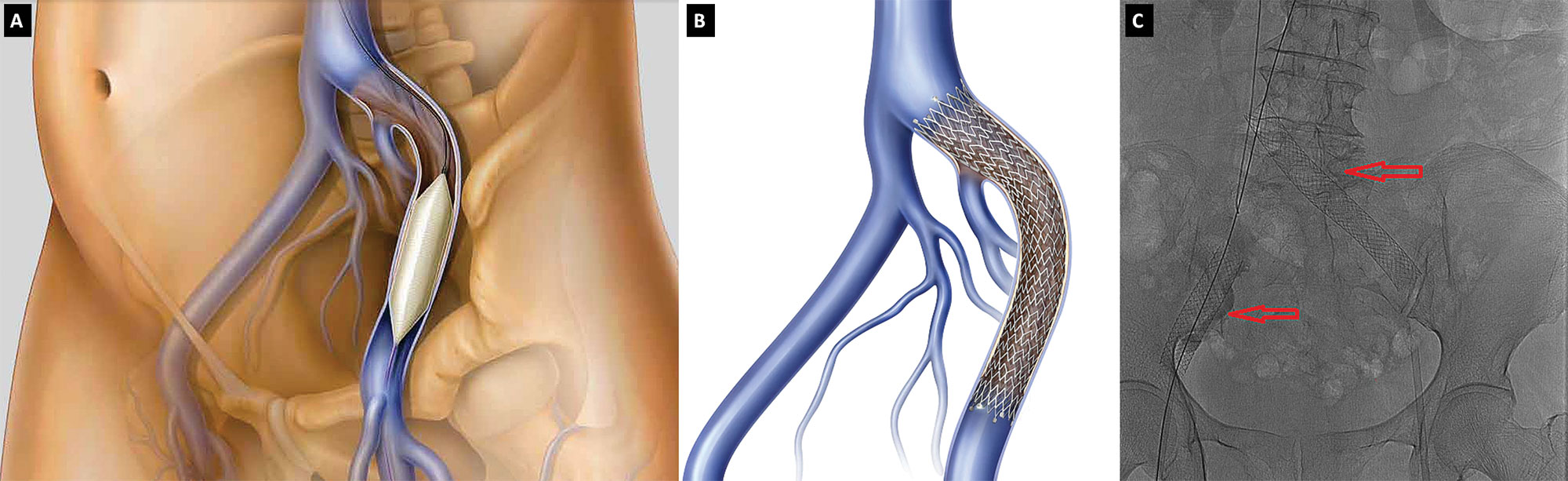
Once your physician or non-physician provider determines that you have iliac vein compression syndrome, treatment is aimed first at improving symptoms. This can be done with use of compression stockings, leg elevation, frequent walking, avoiding prolonged periods of standing, and maintaining a healthy weight. Occasionally, medications to reduce swelling are useful. Severe symptoms can be treated with a stent placed inside the vein where it is compressed during a procedure much like a diagnostic venogram. This can sometimes cause low back pain lasting for a couple of days to a week after the procedure.
- Drawing illustrating a balloon expanded inside an iliac vein (©Becton Dickinson. Used with permission). B. Stent placement in the left common and external iliac veins (©Becton Dickinson. Used with permission). C. Stents (red arrows) in the right and left common iliac veins in a patient (The Healthy Veins Book, 2023, p. 179, fig. 34-5).
Chapter 34: Deep Vein Blockage in the Pelvis: May-Thurner Syndrome