January/February Issue of Vein Specialist
Vascular Verification: Where are We Now and When Will It Involve the Vein World?

Anil Hingorani, MD
Member, AVF Newsletter Committee
Member, AVF Membership Committee
Recent investigations and widely publicized articles have shaken the faith of patients, payers, and referring physicians in the safety and indications for vascular procedures. While these have been mostly focused on arterial disease, some suggest that venous care is not exempt from these concerns. How do we maintain the integrity of patient safety and quality when there are no national guidelines for office-based procedures and half of the states do not have any certification process?
In September 2023, the American College of Surgeons and the Society for Vascular Surgery launched the outpatient effort for the Vascular Verification Program (Vascular -VP). Outpatient facility verification demonstrates to patients, referring physicians, regulators, and payers that high quality, high value vascular care is being delivered. Participants who successfully complete the verification process will set the standard for vascular care in their community and become the leaders in quality and safety. This can be an important feature in our increasingly competitive market.
The release of this new set of outpatient standards for the Vascular-VP puts the same emphasis on quality in outpatient settings that has been applied to inpatient settings that we are all familiar with. This is an important step forward as this is the first ACS program focused on the outpatient sphere and acknowledges the growth of our field.
These new Vascular-VP outpatient standards include elements of vascular surgical care and quality across 9 domains, including:
- Institutional commitment
- Program scope and governance
- Resources for facilities, equipment, services, and personnel
- Clinical care
- Data abstraction and analysis
- Quality improvement
All of the programs that have undergone this process have identified the importance of the process of preparation, the site visit, the external review and summary as one of the key benefits. During the process, the entire team comes together to compile all of the pieces of the program to identify strengths and areas for improvement.
Centers interested in becoming verified are encouraged to apply online.
A short video briefly describes the program, why it is important, and how to leverage it. https://www.youtube.com/watch?v=s1mvGF945Yw
So, getting back to the original question of when this will involve the vein world, I would suggest that this already involves the venous field, and the time to consider looking into the standards for the ACS/ SVS Vascular- VP is now.
Defy Gravity Campaign

Margaret Hopkins, BS, MHA
US Marketing Activation Manager, Essity
The Defy Gravity Campaign was born of the question “How can we break the many prejudices and taboos surrounding compression?” Many patients feel that living a “normal” life is difficult when you feel weighed down by a condition both physically and emotionally. With this campaign, we want patients to feel empowered to live the life they want, regardless of their condition. The Defy Gravity Campaign is about changing the societal perceptions of these conditions and normalizing wearing compression garments.
We refuse to let lipedema, lymphedema, or venous conditions remain taboo. That is why we brought together a group of fearless individuals who defied the limitations of their condition by trying synchronized swimming for the first time. Through their inspiring stories, we aim to show that nothing can hold you down.

Asking real patients of JOBST® to share their most intimate stories about living with their disease was a bold and compelling idea. “Through personal storytelling, ripe with honesty and humor, we learn how someone builds and lives a vibrant life in spite of their disease because JOBST® can improve lives and empower people around the world to ‘defy gravity,’” commented Michaela Tebroke, Global Therapeutic Area Director Compression Therapy, GMI.
This campaign chose synchronized swimming–a sport usually focused on perfection–to redefine the idea of perfection. The ambassadors, all real patients, took to the pool showcasing a defiant performance and a beautiful representation of venous and lymphatic patients “defying gravity.”
We hope their stories will inspire others to seek a diagnosis and to not be ashamed or embarrassed of their condition.
Breaking barriers for venous and lymphatic patients since 1950.
To learn more, visit DEFY GRAVITY (jobst-usa.com)

Industry Collaboration: The Importance of Industry for Meeting Unmet Clinical Needs

Shon Chakrabarti, M.D., M.P.H.
Chief Medical Officer, LimFlow and Former General Manager, Chronic Venous Therapies

Craig Markovitz, Ph.D.
Vice President, Clinical Affairs, Inari Medical
Many patients continue to suffer from limited treatment options and stagnant outcomes across various diseases like deep vein thrombosis (DVT) and chronic venous disease, highlighting the pressing necessity for innovative therapy development and assessment. Industry professionals play a crucial role in pioneering novel therapies. Collaborating with visionary physicians, industry engineering and scientific experts drive the creation of breakthrough technologies that can shift treatment paradigms. Additionally, industry can provide substantial financial, regulatory, and administrative resources required for research and implementation of new technologies—resources typically unavailable within clinical institutions, thus impeding timely advancements. While funding from bodies like the National Institutes of Health is esteemed for its objectivity and prestige, there is insufficient funding available from public granting institutions to satisfy all the needs of the medical community. Physicians committed to advancing care for their patients, along with patients eagerly anticipating progress, cannot afford to disregard the agile industry resources and collaboration.
A good example of industry partnering with clinicians to provide progressive treatments is happening now within the DVT disease state. Patients suffering from DVT have limited treatment options, with debilitating complications and suboptimal effectiveness. Residual thrombus can lead to pulmonary embolism and post-thrombotic syndrome with diminished quality of life1, increased health care costs2, and complications including recalcitrant venous leg ulcers3. The ClotTriever System (Inari Medical, Irvine, CA), FDA-cleared in February 2017, offers lytic-free DVT thrombus removal without associated bleeding risks. Innovations like ClotTriever Bold for chronic material extraction and ClotTriever XL for large vessel thrombus removal further showcase Inari’s commitment to advancing DVT treatment. Additional new products, including Protrieve for IVC thrombus capture in complex DVTs and RevCore for acute-to-chronic in-stent venous occlusions, are designed to enhance outcomes for challenging cases (Fig. 1). A case example of in-stent occlusion clearance with RevCore is shown in Fig. 2.
As important as developing new technology for unmet clinical needs is, the generation of clinical data to investigate the safety and effectiveness of these new products is critical. Industry can provide significant and agile resources for the design, execution, and analysis of much-needed studies for evidence generation. Using DVT again as an example, the ongoing multicenter, prospective CLOUT registry is evaluating 500 DVT patients treated with ClotTriever with 2 year-follow-up to collect long-term patient-centric outcomes.4 To compare ClotTriever outcomes to the current standard of care, Inari has also initiated the DEFIANCE randomized controlled trial (Fig. 3).
Robust evidence from clinical studies including large registries and randomized controlled trials will not only help support emergent therapies, but it can also impact timely and much-needed updates in treatment guidelines. These clinical investigation efforts, alongside the development of 4 new and purposeful DVT thrombectomy tools within 6 years, testify to industry’s ability and commitment to address clinical needs. The recent surge in endovascular products from myriad device companies underscores industry’s eagerness and dedication to bridge gaps in patient care. Inari Medical’s commitment to innovation remains unwavering into 2024 and beyond, as it continues groundbreaking work to provide unique solutions to patients with unmet clinical needs.
References
- Kahn SR, Comerota AJ, Cushman M, Evans NS, Ginsberg JS, Goldenberg NA, et al. The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2014;130(18):1636-61.
- Ashrani AA, Heit JA. Incidence and cost burden of post-thrombotic syndrome. J Thromb Thrombolysis. 2009;28(4):465-76.
- Kahn SR, Solymoss S, Lamping DL, Abenhalm L. Long-term outcomes after deep vein thrombosis: Postphlebitic syndrome and quality of life. 2000. J Gen Intern Med. 15:425-429.
- Bisharat MB, Ichinose EJ, Veerina KK, Khetarpaul V, Azene EM, Plotnik AN, et al. One-year clinical outcomes following mechanical thrombectomy for deep vein thrombosis: a CLOUT registry analysis. JSCAI. 2024; accepted for publication.
Figure 1: Innovative Toolkit for Treatment of Acute-to-Chronic Deep Vein Thrombosis
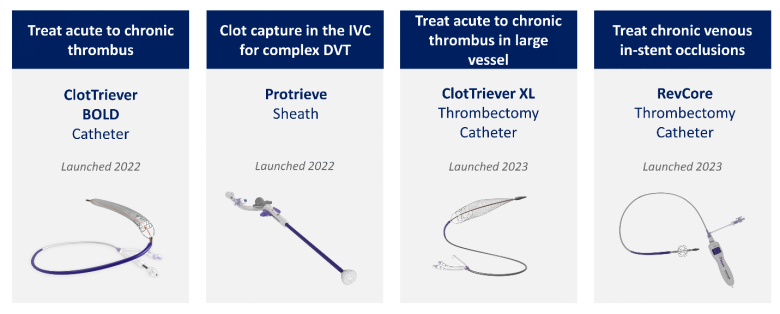
IVC: inferior vena cava; DVT: deep vein thrombosis
Figure 2: Representative Case of an Occluded Stent Thrombectomy Using RevCore, ClotTriever, and Protrieve. A: Pre-thrombectomy venogram showing occluded left iliac stents (arrows). B. Peri-procedural venogram showing thrombus entrapped within Protrieve device placed in the IVC (arrow). C: Post-thrombectomy venogram demonstrating non-occluded stent. D: Example of extracted thrombus within RevCore struts. E: Extracted thrombus post-RevCore and post-16Fr ClotTriever thrombectomy. Case images provided by Dr. Arun Jagannathan, Central Illinois Radiological Associates, Kankakee, IL.
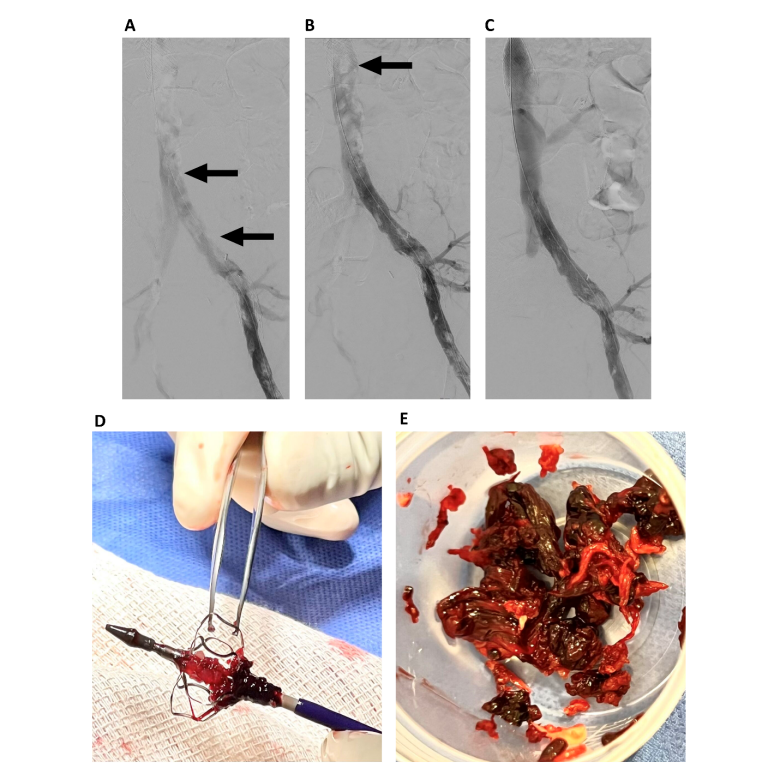
Figure 3: Current Inari-sponsored Deep Vein Thrombosis Studies
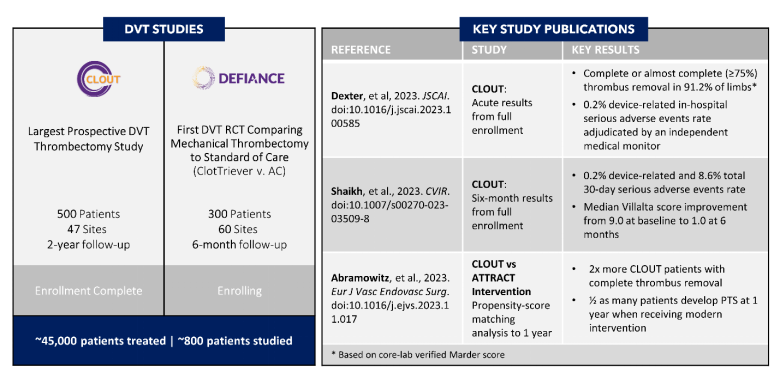
DVT: deep vein thrombosis; RCT: randomized controlled trial; AC: anticoagulation; PTS: post-thrombotic syndrome
FIGURE LEGENDS
Figure 1: Innovative Toolkit for Treatment of Acute-to-Chronic Deep Vein Thrombosis. IVC: inferior vena cava; DVT: deep vein thrombosis
Figure 2: Representative Case of an Occluded Stent Thrombectomy Using RevCore, ClotTriever, and Protrieve. A: Pre-thrombectomy venogram showing occluded left iliac stents (arrows). B. Peri-procedural venogram showing thrombus entrapped within Protrieve device placed in the IVC (arrow). C: Post-thrombectomy venogram demonstrating non-occluded stent. D: Example of extracted thrombus within RevCore struts. E: Extracted thrombus post-RevCore and post-16Fr ClotTriever thrombectomy. Case images provided by Dr. Arun Jagannathan, Central Illinois Radiological Associates, Kankakee, IL.
Figure 3: Current Inari-sponsored Deep Vein Thrombosis Studies. DVT: deep vein thrombosis; RCT: randomized controlled trial; AC: anticoagulation; PTS: post-thrombotic syndrome