September/October Issue of Vein Specialist
Innovations in Venous Wound Care:
Emerging Technologies

Alisha Oropallo, MD, FACS, FSVS, FAPWCA, FABWMS
Professor of Surgery, Zucker School of Medicine, Hofstra/Northwell
Professor, Feinstein Institutes for Medical Research
Program Director, Wound and Burn Fellowship, Northwell Health
Director, Department of Vascular and Endovascular Surgery
Comprehensive Wound Healing Center and Hyperbarics, Northwell Health
Chronic wounds, particularly those associated with venous insufficiency, represent a significant challenge in healthcare. However, the landscape of wound care is undergoing a transformative shift, thanks to the emergence of new and innovative technologies that offer renewed hope for patients and clinicians alike.
Recent additions to negative pressure wound therapy such as instillation and dwell time (NPWTi-d) have revolutionized wound care. Mechanical debridement performed with NPWTi-d with this additional feature has allowed for improvements in wound hygiene (1). The solution of choice–whether antiseptic or not–has given clinician options to personalize the care.
Bioengineered skin substitutes, cellular acellular matrix-like products, have emerged as a significant change in wound management. These innovative products, derived from human cells, animal sources, or synthetic materials, offer a temporary or permanent replacement for damaged skin. They play a role in wound closure, scar reduction, preparing the wound bed for skin grafting or flap placement, and overall healing. The advent of 3D printing and bioprinting has brought in a new era of possibilities in wound care. These skin patches may also be involved with drug delivery (2). Custom-fit wound dressings, scaffolds for tissue regeneration, and even bio-printed skin grafts are being actively explored as potential applications.
Stem cell therapies and growth factor injections are under investigation as potential treatments for chronic wounds. Stem cells, with their unique ability to differentiate into various cell types and promote tissue regeneration, offer the potential to revolutionize the treatment of chronic wounds. Research is ongoing to explore the use of stem cells derived from various sources, such as bone marrow, adipose tissue, and umbilical cord blood, in promoting wound healing and tissue repair (3).
Platelet-rich plasma (PRP) therapy has gained recognition as a promising adjunct in wound healing. PRP is autologous and contains a concentrated number of platelets, growth factors, and cytokines that play a role in tissue repair and regeneration. When applied to chronic wounds, PRP can potentially accelerate healing, reduce inflammation, and improve tissue quality (4).
Electrical stimulation (ES), delivered through electrodes placed around the wound, has shown potential in enhancing blood flow, mitigating inflammation, and stimulating tissue repair. ES is non-invasive and applies a low-level electrical current to the wound area, stimulating cellular activity, promoting angiogenesis, and enhancing tissue perfusion. This can lead to improved wound healing, reduced inflammation, and decreased pain (5). Various forms of ES, such as direct current and pulsed current, are being investigated for their potential benefits in managing chronic wounds.
While many of these technologies are still in their early stages, the rapid pace of research and development suggests that a new era of wound care for venous leg ulcers is emerging. These innovations may offer improvement in healing outcomes while personalizing the care rendered.
References
- Lee P. Treating fasciotomy wounds with negative pressure wound therapy with instillation and dwell time (NPWTi-d). Cureus. October 28, 2016. doi:10.7759/cureus.852
- Jiahui He, Yuyue Zhang, Xinge Yu, Chenjie Xu. Wearable patches for transdermal drug delivery, Acta Pharmaceutica Sinica B, Volume 13, Issue 6, 2023, 2298-2309,
doi:10.1016/j.apsb.2023.05.009
- Rodriguez J, Boucher F, Lequeux C, et al. Intradermal injection of human adipose-derived stem cells accelerates skin wound healing in nude mice. Stem Cell Research and Therapy. 2015;6(1). doi:10.1186/s13287-015-0238-3
- Khan A. Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF). In: Regenerative Medicine in Aesthetic Treatments. CRC Press; 2021:61-66. doi.org/10.1201/9781003001478-8
- Haesler E. Electrical stimulation therapy for wound-related pain: a WHAM evidence summary. Wound Practice and Research. 2024;32(2). doi:10.33235/wpr.32.2.108-112
Lymphedema of Venous Etiology and Venous Leg Ulcers:
Achieving Accelerated Outcomes

M. Mark Melin, MD
Gonda Vascular Center, Wound Clinic
Mayo Clinic, Rochester, MN

Monika Glovizcki, MD, PhD

Michael Y. Shao, MD
Carmel and Fishers, IN
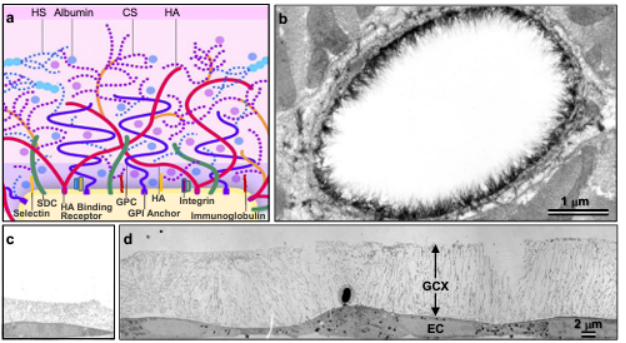
Dogma dies hard, and the classic Starling principle describing venous reabsorption of fluid dies even harder. At this point, if Ernst Starling were among us, he potentially would say “where is your intellectual curiosity? My data is from 1896! Wake up!” The discovery of the endothelial glycocalyx resulted in creation of the revised Starling principle, emphasizing that 90% of fluid is transported via lymphatics and not via reabsorption into the venules (Figure 1) (1-3). The glycocalyx has E-P-I-C functionality (Endothelial cell function [nitric oxide production]; Permeability regulation; Inflammation quenching; Coagulation regulation). Recognition of the importance of permeability regulation has resulted in the renaissance of lymphatic recognition, lymphatic research, and the determination of pathophysiologic contributions to chronic venous insufficiency; specifically, the shedding of venous endothelial glycocalyx components due to altered shear forces associated with venous hypertension. Near InfraRed Fluorescence imaging (NIRFLI) with intradermal indocyanine green has clearly demonstrated the dermal lymphatic dysfunction from early venous disease to C6 status(4). The glycocalyx is now recognized to exist within not only veins and arteries but also the lymphatic vasculature (5). Venous leg ulcerations are the result of dual system failure (both venous and lymphatic) (6). Educational discussions may benefit from discussing the CLEF model (Congestive Lower Extremity Failure) (7), which is analogous to congestive heart failure (CHF) and its pulmonary impact. CHF is a condition that 2nd year medical students can readily describe. We need to enhance education to the same level for CLEF given its extensive prevalence.
With the growing incidence of diabetes and arterial diseases, mixed venous ulcerations are now more prevalent. Hence performance of ankle-brachial indices as a standard component of lower extremity venous ulceration evaluation should be contemplated and further researched in depth. Data demonstrate that compression in mixed venous ulcerations is not contraindicated and should be a standard of care when applied accurately (8). Initially counterintuitive from the perspective of lymphatic functionality, stimulation of dermal lymphatics improves interstitial edema management, hence improving microvascular arterial perfusion. More research is needed in this critical area regarding the management of diabetic foot ulcers, as hyperglycemia has also been recognized to shed the endothelial glycocalyx resulting in increased interstitial edema that compromises diabetic foot ulcer healing (9).
While ablation of axial reflux has been widely accepted as a mainstay in the treatment of VLUs, recent data suggest that for recalcitrant VLUs, axial ablation and standard local wound care alone may not be sufficient and that targeting the terminal refluxing tributaries may achieve accelerated ulcer healing and lower recurrence rates. The multicenter VIEW-VLU study (10) demonstrated that in a challenging patient population (mean BMI 36.3, starting median ulcer size of 6.4 cm2, and mean ulcer age of 8.7 months), treatment of both the axial saphenous reflux and refluxing tributaries using 1% polidocanol endovenous microfoam can achieve impressive healing rates and low recurrence rates. In this difficult wound population, treatment with 1% polidocanol endovenous microfoam resulted in a 53.8% heal rate at 12 weeks with a median healing time of 89 days. 87% of the healed ulcers remained closed 1 year after healing. Although further randomized studies are needed, the VIEW-VLU trial suggests that ablation of the terminal refluxing tributaries leading to the ulcer bed speeds wound healing and reduces recurrence (10).
Micronized Purified Flavonoid Fraction (MPFF, a micronized bioflavonoids supplement composed by diosmin and hesperidin fraction) has the inhibition of leucocyte activation and adhesion as a main mechanism of action (11, 12). Its pharmacologicproperties include,among others, anti-inflammatory and antioxidant activity, increased venous tone, decreased capillary permeability, microcirculatory protective effects, and improved lymphatic drainage. In addition, some data suggest its utility specifically in diabetic microangiopathy. Several RCTs and meta-analyses demonstrated MPFF’s value in the management of venous leg ulcers (VLUs) as adjunctive to compression therapy and local wound care(11). MPFF is recognized as an ancillary VLU treatment by the guidelines of many scientific societies, such as American Venous Forum, Society for Vascular Surgery, and Wound Healing Society (13).
Changing the dogma of current venous leg ulceration management involves teaching the elements of the revised Starling principle with appropriate recognition of endothelial glycocalyx function (1,2); the critical nature and importance of lymphatic function and stimulation to soft tissue regeneration and healing; early and complete venous therapies; adjunctive therapies such as well-evidenced use of micronized purified flavanoid fraction; and the recognition of the growing prevalence of mixed venous-arterial disease. Simply ablating and sclerosing veins is no longer fully adequate if we are to accelerate outcomes, decrease recidivism, decrease expensive skin substitute use, and mitigate the rising overall cost of care. The paradigm shift starts with our collective servant leadership through reading, understanding, and teaching these principles to the next generation.
Figure 1
Mayo Clinic, Rochester, MN created image, all rights reserved, June 2024
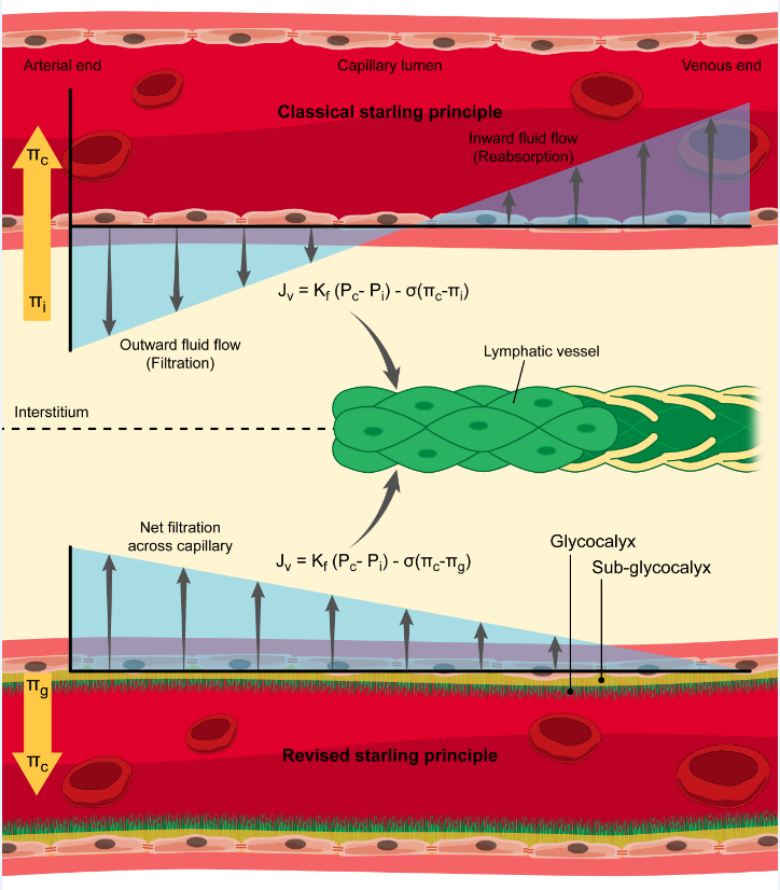
Figure 2. © 2017. Mitra R, O’Neil GL, Harding IC, et al. (3). Used with permission.
References
1 Mortimer PS, Rockson SG. New developments in clinical aspects of lymphatic disease. J Clin Invest. 2014 Mar;124(3):915-21. doi: 10.1172/JCI71608. Epub 2014 Mar 3. PMID: 24590276; PMCID: PMC3938261.
2 Foote CA, Soares RN, Ramirez-Perez FI, et al. Endothelial glycocalyx. Compr Physiol. 2022 Aug 23;12(4):3781-3811. doi: 10.1002/cphy.c210029. PMID: 35997082; PMCID: PMC10214841.
3 Mitra R, O’Neil GL, Harding IC, et al. Glycocalyx in atherosclerosis-relevant endothelium function and as a therapeutic target. Curr Atheroscler Rep. 2017 Nov 10;19(12):63. doi: 10.1007/s11883-017-0691-9. PMID: 29127504; PMCID: PMC5681608.
4 Rasmussen JC, Zhu B, Morrow JR, et al. Degradation of lymphatic anatomy and function in early venous insufficiency. J Vasc Surg Venous Lymphat Disord. 2021 May;9(3):720-730.e2. doi: 10.1016/j.jvsv.2020.09.007. Epub 2020 Sep 22. PMID: 32977070; PMCID: PMC7982349
5 Gianesini S, Rimondi E, Raffetto JD, et al.. Human collecting lymphatic glycocalyx identification by electron microscopy and immunohistochemistry. Sci Rep. 2023 Feb 21;13(1):3022. doi: 10.1038/s41598-023-30043-x. PMID: 36810649; PMCID: PMC9945466.
6 Farrow W. Phlebolymphedema-a common underdiagnosed and undertreated problem in the wound care clinic. J Am Col Certif Wound Spec. 2010 Apr 22;2(1):14-23. doi: 10.1016/j.jcws.2010.04.004. PMID: 24527138; PMCID: PMC3601853.
7 Chuback JA, Melin MM, Massey HT, Gloviczki ML. Congestive lower extremity failure: An educational model for improved understanding of phlebolymphedema. J Vasc Surg Venous Lymphat Disord. 2024 Mar;12(2):101737. doi: 10.1016/j.jvsv.2023.101737. PMID: 38368030.
8 Mosti G, Cavezzi A, Bastiani L, Partsch H. Compression therapy is not contraindicated in diabetic patients with venous or mixed leg ulcer. J Clin Med. 2020 Nov 19;9(11):3709. doi: 10.3390/jcm9113709. PMID: 33227909; PMCID: PMC7699243.
9 Dogné S, Flamion B, Caron N. Endothelial glycocalyx as a shield against diabetic vascular complications: involvement of hyaluronan and hyaluronidases. Arterioscler Thromb Vasc Biol. 2018 Jul;38(7):1427-1439. doi: 10.1161/ATVBAHA.118.310839. Epub 2018 Jun 7. PMID: 29880486; PMCID: PMC6039403.
10 Shao MY, Harlin S, Chan B, et al. VIEW-VLU Investigators. VIEW-VLU observational study of the effect of Varithena on wound healing in the treatment of venous leg ulcers. J Vasc Surg Venous Lymphat Disord. 2023 Jul;11(4):692-699.e1. doi: 10.1016/j.jvsv.2023.01.011. Epub 2023 Mar 25. PMID: 36972751.
11 Coleridge-Smith P, Lok C, Ramelet AA. Venous leg ulcer: a meta-analysis of adjunctive therapy with micronized purified flavonoid fraction. Eur J Vasc Endovasc Surg. 2005 Aug;30(2):198-208. doi: 10.1016/j.ejvs.2005.04.017. PMID: 15936227.
12 Huwait E, Mobashir M. Potential and therapeutic roles of diosmin in human diseases. Biomedicines. 2022 May 6;10(5):1076. doi: 10.3390/biomedicines10051076. PMID: 35625813; PMCID: PMC9138579.
13 Gloviczki P, Lawrence PF, Wasan SM, et al. The 2023 Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society clinical practice guidelines for the management of varicose veins of the lower extremities. Part II: Endorsed by the Society of Interventional Radiology and the Society for Vascular Medicine. J Vasc Surg Venous Lymphat Disord. 2024 Jan;12(1):101670. doi: 10.1016/j.jvsv.2023.08.011. Epub 2023 Aug 29. PMID: 37652254.
Open Vein Surgery is Not Dead Yet!

John C Lantis II, MD, FACS
Mount Sinai West Icahn School of Medicine

Allegra Fierro, MD
Mount Sinai West and Icahn School of Medicine
While everyone is busy lasering and microwaving veins closed, an indication for “old- fashioned” vein stripping and perforator ligation still exists. When you treat both venous disease and venous ulceration, open surgery becomes even more attractive. Certainly, the evidence is well documented that treating veins not only prevents recurrence of venous ulceration (1), but also diminishes the time to closure (2). Therefore, treating the veins expediently, as well as treating the ulcer concomitantly, allows for rapid closure of the ulcer, and frees the patient from recurrence.
That being said, not all veins are amenable to endovenous therapy. I realize my colleagues who are fans of foam sclerotherapy may disagree with this. However, it only takes a couple patients’ coming to see you for a 2nd or 3rd opinion who are asking about the hard lumps in their legs for you to feel that not all large refluxing veins should undergo foam ablation. In addition, the now-well-recognized issue of worsening of the reflux in the anterior accessory vein and its concomitant lower leg veins often leads to ongoing venous ulceration even after “successful” greater saphenous vein ablation.
Therefore, we find that the open operative intervention gives us an opportunity to provide comprehensive single “surgical” correction of the superficial venous hypertension, while allowing us to debride the open leg ulcer and place a cellular, acellular, or matrix-like product (CAMP) on the ulcer to facilitate closure (Figure 1). It has been very rewardingto find the feeding vein actually terminating directly in the ulcer, which we have seen twice in the last 6 months.
We certainly offer appropriate laser and other ablative therapy. However, for the young patient who has severe greater saphenous vein reflux and/or small saphenous vein reflux, we definitely consider surgical intervention to treat the venous hypertension in the lower extremity, including incompetent perforators and the ulcer, all at one time. The number of patients we see who have ongoing ulceration despite previous “successful” venous ablation is significant. Therefore, their tortuous veins and incompetent perforators have often not been treated at all.
The pre-operative process involves an extensive lower leg physical exam of the patient while standing and pre-operative ultrasound to mark the incompetent perforators and the hard-to-visualize or -palpate superficial refluxing veins, especially in the peri-wound area. Excision and ligation of multiple refluxing veins is the norm, with ligation under direct visualization of incompetent perforators, and closure of the skin including skin glue. After this is carried out, we move to the dirty procedure: the venous ulcer is widely excised or at least excised with tangential hydro surgery, and subsequently covered with a CAMP. It is true that peri-ulcer veins may at times be better treated with local sclerotherapy after proximal surgical correction, so this is done at a separate sitting.
In closing, surgical intervention allows for comprehensive closure with minimal risk and rapid return to function when done correctly. Treating the underlying pathophysiology and the patient’s chief complaint at the same time is very rewarding to the patient and to the surgeon.
References
- Barwell JR, Davies CE, Deacon J, et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet. 2004 Jun 5;363(9424):1854-9.
- Gohel MS, Heatley F, Liu X, et al. EVRA Trial Investigators. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018 May 31;378(22):2105-2114.